Past Issues
Mother in Me (MiM): A Prevention and Early Intervention Program in Perinatal Depression – A Pilot Trial
Mariana Vaz Marques1,2,3,*, Julieta Azevedo1,2, Sandra Xavier1,2, Frederica Carvalho1, António Macedo1,3,4, Ana Telma Pereira1,4
1Institute of Psychological Medicine, Faculty of Medicine, University of Coimbra, Portugal
2Center for Research in Neuropsychology and Cognitive Behavioral Intervention (CINEICC), University of Coimbra, Portugal
3Coimbra Hospital and University Centre (CHUC), Coimbra, Portugal
4CIBIT Coimbra Institute for Biomedical Imaging and Translational Research
*Corresponding author: Mariana Vaz Marques Institute of Psychological Medicine, Faculty of Medicine, University of Coimbra, Rua Larga, 3004-504, Coimbra, Portugal. Email: [email protected]
Received: November 29, 2022
Published: December 09, 2022
Citation: Vaz Marques M, et al. (2022). Mother in Me (MiM): A Prevention and Early Intervention Program in Perinatal Depression – A Pilot Trial. Cases. 1(1):5.
Copyright: Vaz Marques M, et al. © (2022).
ABSTRACT
Cognitive behavioral therapies and mindfulness training during pregnancy have already been recognized as important tools in improving perinatal mental health [1]. Nevertheless, further randomized controlled trials (RCTs) are needed [2]. This study aimed to test the efficacy of Mother in Me (MiM), a prevention/ early intervention program for perinatal depression in a pilot RCT.
32 women with depressive symptomatology and/or risk factors for perinatal depression were randomly assigned to two experimental groups (EG - MiM 8-sessions) or equivalent control groups (Treatment as Usual-TAU), filling a set of self-report questionnaires to assess psychological distress, self-compassion and mindfulness at baseline (T0 - during pregnancy), at post-intervention (T1) and at 5-weeks postpartum (T2).
Pre/post-intervention scores showed a decrease in depressive symptoms, negative affect and antenatal anxiety, as well as an increase in self-compassion (EG). In the postpartum, we found that 50% of the participants improved from the depressive symptoms and that 40% experienced a decrease in negative affect. Qualitative results supported the perceived benefits of mindfulness and self-compassion.
Even though our results were not as expressive as we might expect, there was a clinically reliable improvement in depressive symptoms in half of the experimental group. This encourages the team to improve the MiM, which is our next step, conducting a new RCT with the improved program. Keywords: perinatal depression; prevention; early intervention; pilot randomized controlled study.
Keywords: perinatal depression; prevention; early intervention; pilot randomized controlled study
INTRODUCTION
Pregnancy and the first postnatal year are periods of considerable physiological and psychological changes requiring substantial adjustments in a woman’s life, which increases their vulnerability to developing major depression [3]. For this reason, perinatal depression is considered an important public health problem [4], and particularly in Portugal, has shown a prevalence of 4.9% of Major Depressive Disorder (MDD) according to DSM-5 postpartum (assessed at approximately seven weeks) and the information regarding validated and adapted programs for perinatal depression is scarce [5]. Due to the regular contact women have with health services during the perinatal period, this constitutes a privileged opportunity for prevention and intervention initiatives [6].
Several psychological interventions designed to prevent postpartum depression effectively lowered levels of postpartum depressive symptoms and decreased the risk for postpartum depressive episodes within 12 months postpartum [6,7]. Our research team found that lower levels of mindfulness and self-compassion abilities in pregnancy were retrospectively associated to a lifetime history of depression [8,9] and prospectively associated to depressive symptoms [10-12], general psychological distress [13] and insomnia [14] in the postpartum. An integrative literature review highlighted the potential effectiveness of cognitive-behavioural therapy (CBT) and mindfulness training during pregnancy to support perinatal mental health, particularly interventions adapted to meet the needs of women in the perinatal period [1]. Another systematic review [2] refers that there is insufficient evidence from high-quality and robust methodological studies to support the recommendation of mindfulness-based programs to promote perinatal mental health. Thus, the authors of this review appealed to the necessity of adequately longitudinal randomized controlled trials, with active controls, to better test the efficacy of these programs. In a more recent systematic review and meta-analysis of randomized controlled trials, although mindfulness-based interventions have shown to be a useful addition to the already existing tools for perinatal women with mental health problems, again, more studies are needed to prove the effectiveness of these interventions, particularly concerning the mental health of women without current mental health problems [15].
The MiM was developed by our research and clinical team to prevent and intervene in perinatal distress by developing alternative and more effective strategies to deal with stress, depressive and anxiety symptoms. The program is completely manualized session by session, and was inspired by previous mindfulness-based intervention programs (that also comprised self-compassion elements) [e.g. MindfulnessBased Childbirth and Parenting [15]; Mindful Motherhood [16], and self-compassion focused [17] since mindfulnessbased interventions seem to reduce psychological distress and increase well-being [2] and prenatal self-compassion predicts lower levels of postnatal depression and anxiety [18].
Furthermore, MiM comprises psychoeducation and is organized in eight weekly sessions of two hours each, starting between the second and third trimester of gestation, and was designed for small groups [8]. A resume of MiM’s components and sessions can be found in Table 1.
|
Presentation (1st session) |
- “Get to know” exercise; - Presentation of the program’s structure and aims. |
|
Psychoeducation/ Cognitive Exercises (1st to 8th session) |
- CBT rational of depression, stress and anxiety (and specificities of the perinatal period); Transition to parenthood, benefits of mindfulness in daily life and in the perinatal period; - Three elements of experience (thoughts, emotions, sensations); - The Observing/mindful self (that is aware of the three elements); - The attitudinal foundations of mindfulness practice; - Childbirth: fear and pain; Acceptance (while exploring daily difficulties); - Emotions and the body; Mastery/pleasurable activities; - People/activities to hold on and to let go; Self-compassion. |
|
Mindfulness and Self-compassion exercises (1st to 8th session) |
|
|
Support Material to session, to take home and homework
(1st to 8th session)
|
|
|
Material available in the room |
|
The group facilitator is expected to have already formal training in contemplative practices and experience in the application of mindfulness-based programs, and further knowledge of self-compassion. The MiM manual is very detailed, allowing other certified professionals to apply the program by clarifying all the steps, materials and scripts for all the exercises and meditations. It also contains a description of what the professional should present/discuss. In appendix, the meditation/mindfulness exercises scripts can be found, as well as the handouts (with complementary theoretical material), homework description sheets and homework registration sheets (one for each session). The manual also contains a CD with all the audio material needed for the participants to do their homework.
Our program distinguishes itself from other programs because it combines cognitive-behavioural elements with mindfulness and self-compassion practices, whereas other programs focus mainly on mindfulness exercises (those applied during pregnancy and those applied at postpartum). The combination of mindfulness and self-compassion practices with cognitivebehavioral elements is considered a major strength since the NICE guidelines recommend psychological interventions for women with perinatal depression or anxiety, often in the form of CBT [19] with a meta-analysis of CBT for perinatal depression showing significantly greater reductions of depression in women receiving CBT than controls [7]. Another important strength of MiM, in comparison with other programs/studies (e.g. Woolhouse et al., 2014), is that it combines the effort of preventing perinatal distress and also takes into account early intervention in pregnant women at risk of depression (having at least one risk factor for postpartum depression and/or depressive symptomatology). The MiM is also structured in eight sessions, following the structure of programs based on mindfulness and self-compassion (e.g. MBSR; MBCT; Mindful Self Compassion/MSC; MBCP), contrary to some studies that were only composed by six sessions, [20,21] which seems to be an important aspect concerning the benefits and impact of these programs. There is a scarcity of studies comparing the efficacy of 8 sessions programs with the efficacy of programs with fewer sessions, but there is some evidence favouring the standard programs [22].
We thus hypothesize that the program Mother in Me will provide strategies for managing stress, negative emotions and depressive symptoms, hence contributing to a decrease in general and pregnancy-related anxiety and depressive symptoms, as well as negative affect and an increase in mindfulness and self-compassion skills when compared to women assigned to the control group.
METHODS
The study was approved by the Ethical Committee of the Faculty of Medicine from the University of Coimbra, and a consent form was signed by all participants, guaranteeing the confidentiality of the data and the rights of the participant, presenting and guaranteeing the respect for the Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects.
Participants
A sample of Portuguese pregnant women was recruited at local primary health care centres while waiting for their pregnancy appointments. Some participants were also recruited through flyers and posters left in health care centres, briefly describing the study and inclusion criteria.
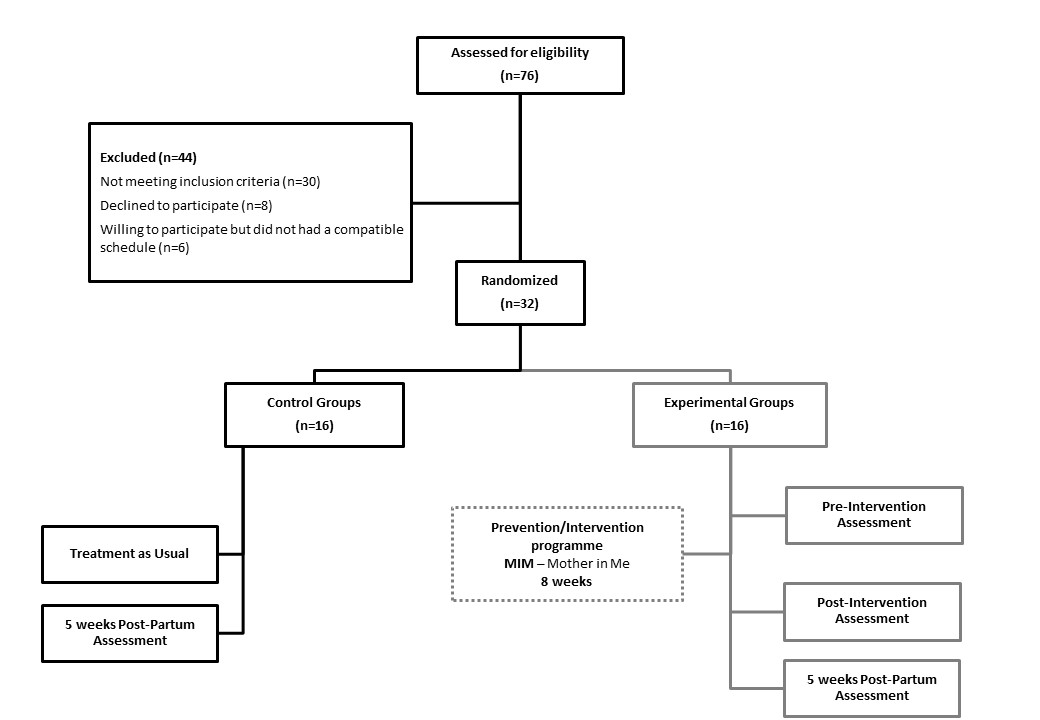
From all the assessed women during pregnancy (recruited between 15 July and December 31), only 76 had the appropriate gestation time to complete the program when contacted to join the experimental group (presenting with a gestation time between 22/28 weeks). From those, 46 participants had the eligibility criteria to participate in the program, and a total of 32 women were accepted to engage in the program (see figure 1 for further detail), being then distributed into control or experimental groups. Of the 16 attributed to the control groups, eight to each, only 4 from group one filled and delivered the questionnaires pre and post-intervention, and later the 5-weeks post-partum assessment, and in the second experimental group, 6 filled and delivered their questionnaires, and attended more than 6 sessions. A total of 10 participants from the experimental groups were then considered for this pilot study, and 15 participants from the control groups, answered all the questionnaires and attended the clinical interview assessments.
Participants (n=25) had a mean age of 31,3 years old (SD=5.54), were in their second trimester (M=22,4 weeks of gestation – measured immediately) and were mainly Portuguese (84%), 48% were married, and 44% were single but all of them were currently living with their partners. Their schooling years varied between 9th grade (4%), high school (more common – 48%), to graduated (40%). Most of the participants were still working when they filled in the questionnaires (60%), some took a leave of absence due to pregnancy (20%), and some were unemployed (16%). There were no significant differences regarding the sociodemographic variables when comparing between control and experimental groups.
Procedure
After being recruited, participants completed the baseline questionnaires where they stated the filing date and the gestation time they were in. After we had around 400 pregnant women, a triage was made to assess how many women had risk factors and/or significant depression symptoms and checked all the eligibility criteria.
The criteria applied for inclusion and exclusion was as follows:
Eligibility Criteria: being pregnant; having between 22 and 30 weeks of gestation – in order to be able to attend the 8-week program; without medical risks associated; could speak and read Portuguese fluently; over the age of 18; willing and able to attend the full 8-week mindfulness course; willing to do postpartum assessment at 5 weeks; willing and able to provide informed consent and having relevant depressive symptomatology and/or one risk factor for perinatal depression (previously identified by our research team, in Portuguese pregnant women: lifetime history of depression, insomnia or negative affect [23].
Exclusion criteria: having experience in meditation; currently attending psychotherapeutic consultations; a history of mental disorders with a dissociative psychotic (e.g. hallucinatory or delusional) component; cannot attend most of the sessions or participate in the subsequent assessments and having 30 weeks of gestation or higher.
The participants of the control and experimental groups were assessed with a semi-structured clinical interview (Diagnostic Interview for Psychological Distress) to assess if any participant was clinically depressed, and they were applied by experienced clinical psychologists.
We considered relevant depressive symptomatology when participants presented PDSS-24 above the cut-off score (above 40), previously established with Portuguese pregnant women [28] and considered the risk factors identified in previous studies [assessed by the Perinatal Depression Screening and Prevention TooL [25]: having a lifetime history of depression, [8] insomnia [26] and/or negative affect (M+SD of Profile of Mood States - POMS-30 score)[27].
All participants filled the same questionnaires at baseline and were then randomly assigned using a computerised randomization system (using SPSS) to either the experimental groups (MiM program) or to the control groups (TAU) [two groups of each (n=8) were created]. The experimental groups were assessed in the week immediately before the program’s first session (Time 0), in order to have a pre-intervention assessment of all participants at the same moment. The control group was assessed at approximately the same gestation time to allow later comparison between groups. Assessment post-intervention (T1) was filled by the experimental groups (immediately after the last session) and again at 5-weeks postpartum by both the control and experimental groups (T2). Screening and eligibility assessment, along with random group distribution presented in Figure 1.
Figure 1. Diagram showing flow of participants and group distribution.
The program Mother in Me was conducted by two clinical psychologists with training in mindfulness and previous experience working in the perinatal period.
Experimental Group
Participants were contacted and informed that they had been selected for the experimental group and they were told when and where the classes would take place (Tuesdays at 6 p.m., at Bissaya Barreto’s Maternity). To attend the sessions, participants received gift cards to cover their transportation expenses. Between sessions, homework assignments were given (daily meditations ranging from 3 to 30 minutes – Table 1) and women were asked to fill home practice register sheets. Participants learned mindfulness meditation practices, including sitting and moving meditations, and how to be with (pleasant or unpleasant) thoughts, emotions and sensations. At the end of the program, participants filled out some evaluation questions and scales, to verify acceptability and to obtain suggestions regarding the program. Women were encouraged to attend all sessions but were considered to have completed the program if they had attended at least six of the eight sessions.
Control group
Women received treatment as usual (TAT) in public health care and did not know that they were assigned to the control group. However, they were informed that if they had not been contacted until their 30th week of pregnancy, they would simply be contacted at 5 weeks postpartum for the postpartum assessment.
Measures
All the participants filled out a battery of self-report questionnaires, validated in a Portuguese sample of pregnant women:
- Perinatal Depression Screening and Prevention Tool – PDSPTool [25-28] which includes: Lifetime History of Depression (LHTD; 20 “Yes/No” questions, based on DSM-5 criteria for depression; 12,13); Insomnia Assessment Scale (IAS; evaluates current insomnia, based on DSM-5 and International Classification of Sleep Disorders, with 14 “Yes/No” questions) [27]; Profile of Mood States (POMS-30; includes 30 items and was used to assess negative affect) [28]; Postpartum Depression Screening Scale (PDSS-24; a shorter form to screen for depression according to ICD-10 criteria) [24];
- Diagnostic Interview for Psychological Distress - Postpartum (DIPD-PP; a new semi-structured clinical interview, based on DSM-5 criteria, assessing Major Depressive Disorder, Anxiety Disorders, Obsessive-Compulsive Disorder and Traumarelated Disorders in the postpartum; (5,30);
- Perinatal Anxiety Screening Scale (PASS) [31]; evaluates stress, anxiety and depressive symptoms, in the last week) [32];
- Self-Compassion Scale (SCS): instrument with 26 items with a 5 point Likert scale to measure self-compassion [33];
- Southampton Mindfulness Questionnaire – 16 (SHQ-16; Measures Mindfulness through 4 distinct components: Mindful Observation (MO) Letting Go (LG), Absence of Aversion (AV) and Non-Judgment (J) [34].
Data analyses
Data was analyzed using SPSS (version 23; SPSS Inc., Chicago, IL). Change scores correcting for measurement error and practice effects were calculated for each participant using Reliable Change Index (RCI) methodology.35 Non-parametric tests were used to analyze differences between groups (control and intervention; Mann-Whitney U and Qui-Square) and to compare intra-group differences across time (Wilcoxon Rank sum test).
The Reliable Change Index (RCI) was calculated for each outcome measure, and this reliable change indicator was used to calculate if there was a significant improvement, no change, or deterioration from pre to post-intervention. A clinically significant change was calculated using the sample means and standard deviations to determine whether or not postintervention scores were reduced to subclinical ranges. Test-retest correlations used in the calculation of reliable change scores were based on Pearson's correlation product moment correlation coefficients. An RCI greater than +1.645 is likely to occur randomly in only 5% of cases (p < .05) and is, thus, considered a significant change, while a reliable decline occurs when values fall below −1.645. Participants were classified as “Improved” or “Deteriorated”, considering these values, which implicate a reliable change [36].
RESULTS
Quantitative analysis
Experimental and control groups were compared at baseline and in the postpartum (5 weeks post-partum), and no significant differences were found. When assessing differences pre and post-intervention with the Wilcoxon sign rank-test, no differences were found neither between baseline and postintervention nor inter-group differences when comparing the 2 experimental groups. An analysis of subject-by-subject pre vs post-intervention scores was performed using RCI, and results from pre-post intervention assessment are summarized in Table 2. Clinically reliable improvement was found in the post-intervention assessment in 10% regarding depressive symptoms, with most participants remaining unchanged (80%). A reliable clinical improvement in negative affect (POMS-NA) was found in 30% of the participants and in the same percentage regarding antenatal anxiety (see table 2 for further detail).
Table 2. Reliable Change Index (RCI): pre vs. post intervention scores (during pregnancy) – Experimental Groups
|
|
Reliable Change Index - Pre-Post Intervention |
||||||
|
Participants |
PDSS-24 Total |
SHQ Total |
SHQ_AV |
POMS-NA |
SCS Total |
SCS_SK |
PASS Total |
|
Subject 1 |
-1.83 UC |
0.24 UC |
0.28 UC |
-0.96 UC |
-0.83 UC |
0.0 UC |
-1.09 UC |
|
Subject 2 |
0.61 UC |
-0.96 UC |
1,12 UC |
-0.72 UC |
1.17 UC |
0.46 UC |
-0.43 UC |
|
Subject 3 |
5.18 Imp |
0.24 UC |
0,28 UC |
0.0 UC |
-2.00 Imp |
-0.93 Imp |
-0.43 UC |
|
Subject 4 |
0.30 UC |
-0.48 UC |
0.56 UC |
0.96 UC |
0.17 UC |
2.32 Imp |
3.69 Imp |
|
Subject 5 |
-0.61 UC |
-2.51 Imp |
-1.97 Imp |
3.12 Imp |
-0.33 UC |
-1.39 UC |
-0.22 UC |
|
Subject 6 |
0.91 UC |
-0.36 UC |
0.00 UC |
2.16 Imp |
-2.16 Imp |
-0.46 UC |
0.87 UC |
|
Subject 7 |
-0.30 UC |
-5.14 Imp |
0.0 UC |
1.44 UC |
1.00 UC |
0.93 UC |
0.43 UC |
|
Subject 8 |
1.82 UC |
-1.56 UC |
-1.69 UC |
5.52 Imp |
-0.33 UC |
0.0 UC |
2.61 Imp |
|
Subject 9 |
-6.71 Det |
2.15 Det |
0.84 UC |
-6.71 Det |
1.33 UC |
2.79 Det |
-1.52 UC |
|
Subject 10 |
0.30 UC |
-1.20 UC |
-0.56 UC |
-0.72 UC |
-0.33 UC |
-1.86 UC |
4.34 Imp |
|
Improved |
10% |
20% |
10% |
30 % |
20% |
20% |
30% |
|
Unchanged |
80% |
70% |
90% |
60% |
70% |
70% |
70% |
|
Deteriorated |
10% |
10% |
0% |
10% |
0% |
10% |
0% |
RCI = Reliable Change Index; PDSS – Perinatal Depression Screening Scale; SHQ – Southampton Mindfulness Questionnaire; AV – Absence of Aversion; POMS NA = Profile of Mood States - Negative Affect; SCS = SelfCompassion Scale; SK – Self-Kindness; PASS - Perinatal Anxiety Screening Scale; Imp – Improved; UC – Unchanged; Det - Deteriorated
Participants from the experimental group that showed improvements, when compared with the participants that did not show improvements or deteriorated, reported weekly practice duration (of mindfulness and self-compassion exercises) from thirty minutes to one hour.
At the postpartum assessment (5th week), 50% of the participants presented an improvement in depressive symptoms (compared with the post-intervention assessment T1 and T2), a reliable improvement in 40% of participants regarding anxiety (PASS) and an improvement in 30% regarding positive affect levels. There was an improvement in 40% of the participants in negative affect and a deterioration in 20% of them (particularly the item regarding fatigue).
After assessing the participants from the experimental group with the semi-structured interview, two confirmed Major Depression diagnoses (corresponding to 20%), and 8 did not present any mental health diagnosis. In the control group, 5 of the 15 participants presented were confirmed with Major Depressive Disorder in the Postpartum, corresponding to a percentage of 33,3%.
Qualitative analysis
Overall, qualitative feedback was very positive. Some examples of the perceptions evaluated in the final form (postintervention questionnaire) are presented in Table 3.
Table 3. Post-intervention feedback from the experimental groups
|
Examples of questions |
Strongly agree |
Agree |
Neither agree nor disagree* |
|
“I developed new strategies to deal with situation that cause me sadness/anxiety and stress, in a more peaceful and secure way” |
25% |
75% |
0% |
|
“I started to be aware that my thoughts affect my feelings, sensations and behaviors” |
37.5% |
50% |
12.5% |
|
“I learned to be more kind with myself” |
12.5% |
75% |
12.5% |
|
“I would recommend this program to another woman” |
25% |
62,5% |
12.5% |
|
“I have been feeling improvements in my quality of life” |
25% |
75% |
0% |
|
“The strategies I’ve learned will help me prepare for childbirth” |
25% |
75% |
0% |
|
“The facilitators-psychologists were able to create a good relationship with the participants” |
75% |
12,5% |
12,5% |
Summarizing, the majority of the participants agreed or strongly agreed that, with the program, they started to be aware of thoughts, emotions and sensations, developed new strategies to deal with difficult emotions and learned to be kinder with themselves. All the participants expressed the program helped them acquire strategies to prepare them for childbirth and to deal with thoughts, emotions and sensations during childbirth/postpartum.
All the participants from the experimental group at the 5th week postpartum reported that, due to the demands of postpartum, they were not able to continue the formal mindfulness (e.g. body scan) and self-compassion (e.g. selfcompassion break) practices, only maintaining some small moments of informal practice (daily-life mindfulness activities, mainly involving the babies).
Participants’ suggestions for the future were: more sessions and more time for sharing; some sessions with their husband/ partner; additional sessions after giving birth; more investment, during the sessions, on the specific issues of pregnancy and postpartum (e.g. informal practices considering the inclusion of the baby in the postpartum).
DISCUSSION
The preliminary results from our pilot randomized controlled trial point to the pertinence of applying a mindfulnessbased intervention in pregnant women at risk of depression, combined with self-compassion and CBT exercises, evidencing quantitative and qualitative improvements regarding the experimental group enrolled in the Mother in Me/MiM program. These results were more evident when considering the reliable change in each participant, from the pre-program to the post-program (during pregnancy) assessment. In fact, quantitative results regarding pregnancy comparisons showed a decrease in depressive symptoms, negative affect and perinatal anxiety, as well as an increase in self-compassion and mindfulness skills, particularly in those women referring weekly practice duration of mindfulness and self-compassion exercises from thirty minutes to one hour. It is surprising that only one individual’s condition deteriorated, considering they were all at risk and that, usually, anxiety increases when delivery gets closer.
The efficacy of the MiM program for perinatal depression was partially supported, with promising indicators of the early intervention potential with pregnant women at risk of depression (having at least one risk factor for postpartum depression and/or depressive symptomatology). In fact, the decrease in depressive symptoms and negative affect during pregnancy, in the experimental group, suggests that this intervention, based in cognitive-behavioural elements, mindfulness and self-compassion training, confers benefits for perinatal mental health. Pregnancy is a period which imposes several changes, felt by women and by their partners, [16] and a multiplicity of negative maternal and infant outcomes are associated with stress and mood disturbance (in this period). [38,39] these results go in the same direction as the MindBabyBody program [22] which provided evidence on the feasibility of an antenatal mindfulness intervention to reduce psychological distress (particularly anxiety) and to increase mindfulness skills in pregnancy. Likewise, a pilot RCT of Mindfulness Training for Stress Reduction during Pregnancy [21] reported that participants experienced large reductions in anxiety when comparing pre and post-intervention scores. Moreover, the pilot study (non-randomized) from Duncan, [26], which tested the Mindfulness-Based Childbirth and Parenting program, showed statistically significant increases in mindfulness and positive affect, and decreases in anxiety, depression and negative affect in pregnancy (from pre to post-test). Our results go in the same direction, having the particularity of using an instrument specifically developed to assess perinatal depression [the PDSS-24/PDSS-21] [25], thus conferring more accuracy to the screening and the outcomes when comparing to other studies which did not use instruments for the perinatal period. [16,17]. Additionally, a recent study which used a smartphone-based mindfulness training showed to improve maternal perinatal depression in women potentially at risk of perinatal depression in early pregnancy [40].
The decrease in depressive symptoms and negative affect in pregnancy was an important outcomes, particularly considering that these are consistent risk factors for the development of perinatal depression, including postpartum depression. These results also highlight the role that mindfulness and self-compassion exercises might have in improving well-being during pregnancy. Likewise, a recent study which used a mindful self-compassion intervention to prevent postpartum depression (6-week internet-based program) found that the intervention group showed significant improvement in depressive and anxiety symptomss when compared to the control group. Moreover, this group became more mindful and self-compassionate at three months and one year postpartum [41].
The decrease in anxiety and the fact that the post-intervention levels did not worsen (T1) was very positive (30% of the experimental group decreased), considering the proximity of childbirth and the natural progression of pregnancy, which are considered particularly stressful events, namely for women at risk [42].
The results concerning the postpartum assessment (5th week postpartum) showing an improvement in depressive symptoms, and self-compassion, although only in a quarter of the participants can be considered preliminary evidence of the potential preventive effect (regarding postpartum distress) of the MiM. Although being a very different study from ours, an open trial of mindfulness-based cognitive therapy for preventing depressive relapse/recurrence at pregnancy and six months postpartum (excluding women with a major depressive disorder diagnosis were excluded) [40] also showed a significant decrease in depressive symptoms levels during pregnancy and at the postpartum. Our results go in the same direction as these, supporting the potential of mindfulnessbased programs in preventing perinatal depression, but then again, more randomized controlled trials are needed to better clarify this potential.
The qualitative outcomes expanded the quantitative results and strengthened the beneficial effects of the program’s exercises, with the emphasis being placed on women’s narrative, revealing a development of important mindfulness and self-compassion skills, such as being more aware of thoughts and emotions and being able to be more compassionate with themselves while suffering (experiencing unpleasant thoughts, feelings…).
All in all, our results encourage us to improve the MiM program and to re-test it in a wider RCT study. EEA Grants allowed us to derive important clinical implications to improve the MiM and to become more competitive in obtaining funding to continue studying its effectiveness.
One of the obstacles we faced was the capacity to gather a group of pregnant women, at risk of depression, with a gestation time between 22 and 28 weeks, and who had the means and availability to attend the group sessions. The fact that the maternity where we approach the participants receives pregnant women from the whole central geographical area of Portugal contributed to this problem, which made the adhesion to the group intervention harder. From the 76 participants that were assessed for eligibility (gestation time between 22-28 weeks), 44 were excluded (30 because they did not meet the remaining eligibility criteria – risk factors and absence of medical risk/complications in pregnancy; 8 had no interest and 6 were not available or had no means to attend the group session). For future studies, one might consider broadening the inclusion criteria, in order to allow more women to access the group and increase the number of participants.
We expected to find differences between the control group and the experimental group, yet in such small groups and with 2 participants in the experimental group who developed MDD, we understand that the eventual improvements faded when comparing the whole group. However, it encourages us that only 2 participants from a risk group developed MDD in the post-partum, even though we need further studies to see if our program can replicate these results.
Therefore, we are currently preparing a new randomized controlled clinical trial incorporating some inferences from this pilot study and the participant´s suggestions. Although maintaining the eight sessions, we will include a retreat day (to reinforce the practices), more moments of sharing, yoga exercises adapted for pregnancy, as well as several moments focusing on how to incorporate mindfulness and selfcompassion elements in their daily lives during pregnancy and the postpartum. The husband/partner’s presence is suggested and allowed, being encouraged primarily in sessions concerning labour, pain and communication patterns, and we reinforce the use of informal exercises since they are easier to maintain in periods such as pregnancy and postpartum, with such high demands.
FUNDING
This work was financed by the EEA Grants-161SM3 and Fundação para a Ciência e a Tecnologia (FCT), PTDC/DTPPIC/2449/2014
ACKNOWLEDGEMENTS
We thank all the women for participating in this study, as to the professionals from Bissaya Barreto Maternity in Coimbra.
CONFLICTS OF INTEREST
None declared
KEYPOINTS
• Mother in Me (MiM) is a new prevention and early intervention program for perinatal depression, including psychoeducation and cognitive-behavioural, mindfulness and self-compassion exercises.
• MiM manual describes all the activities of each session and the materials that the professional should present/ use/discuss in each session.
• Preliminary quantitative results show that participants enrolled in the MiM decreased depressive symptoms and negative affect, as well as increased positive affect, at post-intervention - five weeks postpartum.
• Qualitative results confirmed the perceived benefits of mindfulness and self-compassion practices in preparing for childbirth and dealing with thoughts, emotions and sensations postpartum.
• Longer meditation practice was associated with lower depressive symptoms.
REFERENCES
1. Lavender TJ, Ebert L, Jones D. (2016). An evaluation of perinatal mental health interventions : An integrative literature review. Women Birth. 29(5):399-406. Available from: http://dx.doi.org/10.1016/j.wombi.2016.04.004
2. Hall HG, Beattie J, Lau R, East C, Biro MA. (2016). Mindfulness and perinatal mental health: A systematic review. Women Birth. 29(1):62–71. Available from: http:// dx.doi.org/10.1016/j.wombi.2015.08.006
3. Munk-Olsen T, Laursen TM, Mendelson T, Pedersen CB, Mors O, Mortensen PB. (2009). Risks and Predictors of Readmission for a Mental Disorder During the Postpartum Period. Arch Gen Psychiatry. 66(2):189-195. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19188541
4. Wisner KL, Chambers C, Sit DKY. (2006). Postpartum depression: a major public health problem. JAMA. 296(21):2616-2618. Available from: http://www.ncbi.nlm. nih.gov/pubmed/17148727
5. Pereira A, Marques C, Xavier S, Azevedo J, Soares M, Bento E, et al. (2017). Prevalence and incidence of postpartum Major Depression (DSM-5) in Portuguese women. In: Postpartum Depression: Prevalence, Risk Factors and Outcomes. New York: Nova Science Publishers. p. 61–84.
6. Sockol LE, Epperson CN, Barber JP. (2013). Preventing postpartum depression: A meta-analytic review. Clin Psychol Rev.33(8):1205-1217.
7. Sockol LE. (2015). A systematic review of the efficacy of cognitive behavioral therapy for treating and preventing perinatal depression. J Affect Disord [Internet].177:7-21 Available from: http://dx.doi.org/10.1016/j. jad.2015.01.052
8. Azevedo J, Bento E, Xavier S, Marques M, Freitas V, Soares MJ, et al. (2016). The role of mindfulness in lifetime history of depression: A study in Portuguese pregnant women. Eur Psychiatry. 33:S625–626.
9. Bento E, Xavier S, Azevedo J, Marques M, Soares MJ, Martins MJ, et al. (2016). The role of self-compassion in lifetime history of depression: A study in Portuguese pregnant women. Eur Psychiatry. 33:S416–417. Available from: http://dx.doi.org/10.1016/j.eurpsy.2016.01.1505
10. Pereira AT, Xavier S, Bento E, Azevedo J, Marques M, Soares MJMJ, et al. (2016). Mindfulness, self-compassion and depressive symptoms in pregnant women. Eur Psychiatry. 33S:S420. Available from: http://linkinghub.elsevier.com/ retrieve/pii/S0924933816015212
11. Azevedo J, Marques M, Xavier S, Bento E, Marques C, Soares MJ, et al. (2017). Mindfulness and Perinatal Depression. In: Postpartum Depression: Prevalence, Risk Factors and Outcomes. p. 25–60.
12. Marques C, Martins M, Marques M, Azevedo J, Bento E, Xavier S, et al. (2017). Self-compassion and perinatal depression. In: Anderson G, editor. Postpartum Depression: Prevalence, Risk Factors and Outcomes. New York: Nova Science Publishers. p. 1–24.
13. Xavier S, Azevedo J, Bento E, Marques M, Soares M, Martins MJJ, et al. (2016). Mindfulness, self-compassion and psychological distress in pregnant women. Eur Psychiatry. 33:S484–485. Available from: http://www.embase. com/search/results?subaction=viewrecord&from=export&id=L72291891%5Cnhttp://dx.doi.org/10.1016/j. eurpsy.2016.01.1775%5Cnhttp://jq6am9xs3s.search. serialssolutions.com/?sid=EMBASE&issn=17783585&id=- doi:10.1016%2Fj.eurpsy.2016.01.1775&atitle=
14. Marques M, Pereira AT, Bento E, Xavier S, Azevedo J, Soares MJ, et al. (2016). Self-compassion and insomnia at pregnancy. Eur Psychiatry. 33:S268. Available from: http:// linkinghub.elsevier.com/retrieve/pii/S0924933816007070
15. Yan H, Wu Y, Li H. (2022). Effect of mindfulness-based interventions on mental health of perinatal women with or without current mental health issues: A systematic review and metaanalysis of randomized controlled trials. J Affect Disord. 305: 102-114. Available from: http:// doi:10.1016/j.jad.2022.03.002
16. Duncan LG, Bardacke N. (2010). Mindfulness-Based Childbirth and Parenting Education: Promoting Family Mindfulness During the Perinatal Period. J Child Fam Stud. 19(2):190–202. Available from: http://www.ncbi.nlm.nih. gov/pubmed/20339571
17. Vieten C, Astin J. (2008). Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: results of a pilot study. Arch Womens Ment Health. 11(1):67–74. Available from: http://link.springer. com/10.1007/s00737-008-0214-3
18. Neff K. (2015). Self-Compassion: The proven power of being kind to yourself. New York: HarperCollins Publishers.
19. Cohen S. (2010). Mindfulness and Self-Compassion in the Transition to Motherhood: A Prospective Study of Postnatal Mood and Attachment. University of Columbia. Available from: http://pqdtopen.proquest.com/ doc/858946838.html?FMT=ABS
20. National Institute for Health and Care Excellence. (2014). Antenatal care for uncomplicated pregnancies. Clin Guidel. 1–55. Available from: https://www.nice. org.uk/guidance/cg62/resources/antenatal-care-foruncomplicated-pregnancies-975564597445
21. Guardino CM, Dunkel Schetter C, Bower JE, Lu MC, Smalley SL. (2014). Randomised controlled pilot trial of mindfulness training for stress reduction during pregnancy. 29(3):334-349. Available from: http://www. ncbi.nlm.nih.gov/pubmed/24180264
22. Woolhouse H, Mercuri K, Judd F, Brown SJ. (2014). Antenatal mindfulness intervention to reduce depression, anxiety and stress: a pilot randomised controlled trial of the MindBabyBody program in an Australian tertiary maternity hospital. BMC Pregnancy Childbirth. 14(1):369. Available from: http://www.ncbi.nlm.nih.gov/ pubmed/25343848
23. Demarzo M, Montero-Marin J, Puebla-Guedea M, Navarro-Gil M, Herrera-Mercadal P, Moreno-González S, etal. (2017). Efficacy of 8- and 4-Session Mindfulness-Based Interventions in a Non-clinical Population: A Controlled Study. Front Psychol. 8:1343. Available from: http:// journal.frontiersin.org/article/10.3389/fpsyg.2017.01343/ full
24. Marques M, Pereira ATA, Bos SC, Maia BR, Soares MJM, Marques C, et al. (2017). Risk Factors for Postpartum Depression: A Dimensional and Categorical Approach. In: Gary Anderson, editor. Postpartum Depression: Prevalence, Risk Factors and Outcomes. New York: Nova Science Publishers.
25. Pereira AT, Bos S, Marques M, Maia B, Soares MJ, Valente J, et al. (2013). Short forms of the Postpartum Depression Screening Scale: as accurate as the original form. Arch Womens Ment Health. 16(1):67–77. Available from: http:// link.springer.com/10.1007/s00737-012-0319-6
26. Pereira A, Xavier S, Azevedo J, Bento E, Marques C, Carvalho R, et al. (2015). Predictive ability of the Perinatal Depression Screening and Prevention Tool – Preliminary results of the dimensional approach. BMC Heal Serv Res. 16(3):17.
27. Marques M, Pereira AT, Azevedo J, Xavier S, Bento E, Soares MJ, et al. (2016). Validation of the insomnia assessment scale – adapted in a community sample of portuguese pregnant women. Eur Psychiatry. 33: S269.
28. Bos SC, Soares M, Marques M, Pereira AT, Amaral A, Azevedo MH, et al. (2013). Measuring negative and positive affect in medical students. In: 22nd World Congress on Psychosomatic Medicine. 82.
29. Xavier S, Azevedo J, Bento E, Marques C, Marques M, Macedo A, et al. (2015). Predictive ability of the Perinatal Depression Screening and Prevention Tool – Preliminary results of the categorical approach. BMC Health Serv Res.16(3):84.
30. Pereira AT, Marques M, Soares MJ, Maia BR, Bos S, Valente J, et al. (2014). Profile of depressive symptoms in women in the perinatal and outside the perinatal period: Similar or not? J Affect Disord.166:71–78.
31. Xavier S, Bento E, Azevedo J, Marques M, Freitas V, Soares MJ, et al. (2015). Diagnostic Interview for Psychological Distress: Description, and experts’ panel evaluation. In: 2nd Biennial Perinatal Mental Health Conference2. Chicago.
32. Pereira AT, Pinto C, Azevedo J, Marques C, Xavier S, Soares MJ, et al. (2019). Validity and Reliability of the Perinatal Anxiety Screening Scale in a Portuguese sample of pregnant women. In: 27th European Congress of Psychiatry, Warsaw.
33. Xavier S, Bento E, Azevedo J, Marques M, Soares MJ, Freitas V, et al. (2016). Validation of the Depression, Anxiety and Stress Scale–DASS-21 in a community sample of Portuguese pregnant women. Eur Psychiatry. 33: S239.
34. Bento E, Xavier S, Azevedo J, Marques M, Freitas V, Soares MJ, et al. (2016). Validation of the self-compassion scale in a community sample of Portuguese pregnant women. Eur Psychiatry. 33: S238.
35. Chadwick P, Hember M, Symes J, Peters E, Kuipers E, Dagnan D. (2008). Responding mindfully to unpleasant thoughts and images: Reliability and validity of the Southampton mindfulness questionnaire (SMQ). Br J Clin Psychol. 47(4):451–455.
36. Woods S, Childers M, Ellis R, Guaman S, Grant I, Heaton R, et al. (2006). A battery approach for measuring neuropsychological change. Arch Clin Neuropsychol. 21(1):83–89. Available from: http://www.ncbi.nlm.nih. gov/pubmed/16169705
37. Parsons TD, Notebaert AJ, Shields EW, Guskiewicz KM. (2009). Application of reliable change indices to computerized neuropsychological measures of concussion. Int J Neurosci. 119(4):492–507.
38. Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, et al. (2013). Effects of perinatal mental disorders on the fetus and child. Lancet. 384(9956):1800–1819.
39. Grigoriadis S, VonderPorten EH, Mamisashvili L, Tomlinson G, Dennis C-L, Koren G, et al. (2013). The Impact of Maternal Depression During Pregnancy on Perinatal Outcomes. J Clin Psychiatry. 74(4):e321–41. Available from: http:// www.ncbi.nlm.nih.gov/pubmed/23656857
40. Sun Y, Li Y, Wang J, Chen Q, Bazzano AN, Cao F. (2021). Effectiveness of Smartphone-Based Mindfulness Training on Maternal Perinatal Depression: Randomized Controlled Trial. J Med Int Res. 23(1): e23410. Available form: http://10.2196/23410
41. Guo L, Zheng J, Mu L, Ye Z. (2020). Preventing Postpartum Depression with Mindful Self-Compassion Intervention. A Randomized Control Study. J Nerv Ment Dis.208: 101-107. http://10.1097/NMD.0000000000001096
42. Biaggi A, Conroy S, Pawlby S, Pariante CM. (2016). Identifying the women at risk of antenatal anxiety and depression: A systematic review. J Affect Disord. 191:62–77. Available from: http://dx.doi.org/10.1016/j. jad.2015.11.014
43. Dimidjian S, Goodman SH, Felder JN, Gallop R, Brown AP, Beck A. (2015). An open trial of mindfulness-based cognitive therapy for the prevention of perinatal depressive relapse/recurrence. Arch Womens Ment Health. 18(1):85–94. Available from: http://link.springer. com/10.1007/s00737-014-0468-x
 Abstract
Abstract  PDF
PDF